Does Medicare Cover Diabetic Supplies? A Simple Guide for NY Residents
The Big Question: Part B vs. Part D
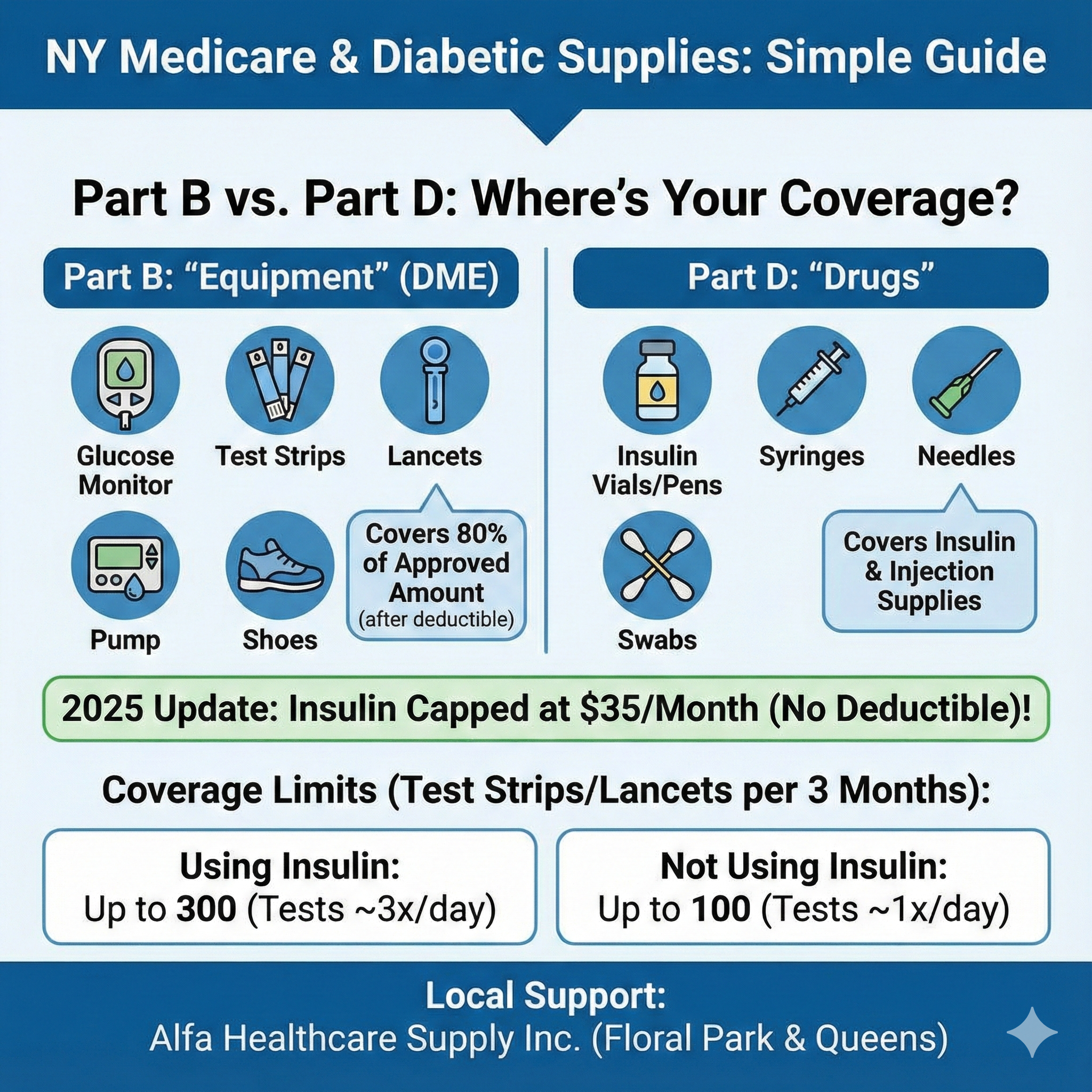
The most common source of confusion is knowing which part of Medicare pays for which item. Medicare doesn’t lump all “diabetic supplies” into one bucket. Instead, they split them based on whether the item is considered “Durable Medical Equipment” (DME) or a medication.
Medicare Part B: The “Equipment” Coverage
Medicare Part B is your medical insurance. It covers outpatient care and, crucially for you, Durable Medical Equipment (DME).
If you have Original Medicare and your doctor prescribes these items for use in your home, Part B typically covers 80% of the Medicare-approved amount (after you meet your deductible). You (or your supplemental insurance) pay the remaining 20%.
Items Covered Under Part B:
- Blood Sugar Monitors (Glucometers): The device used to read your blood sugar.[6]
- Blood Sugar Test Strips: The disposable strips used with the monitor.
- Lancets & Lancet Devices: The spring-loaded device and needles used to draw blood.
- Glucose Control Solutions: Liquid used to check the accuracy of your monitor.
- Therapeutic Shoes & Inserts: Covered if you have diabetic foot complications (specifically for prevention of ulcers).
- Insulin Pumps: If you require a pump, the device and the insulin used in the pump are often covered under Part B as DME.
Medicare Part D: The "Drug" Coverage
Medicare Part D is strictly for prescription drugs. This is usually an add-on plan you purchase separately or part of a Medicare Advantage plan.
Items Covered Under Part D:
- Insulin: Unless used in an insulin pump (see above), insulin is covered here.
- Syringes & Needles: The supplies used to inject insulin manually.
- Alcohol Swabs: Used to clean the injection site.
- Gauze: For post-injection care.
Important 2025 Update: Thanks to the Inflation Reduction Act, the cost of a month’s supply of each covered insulin product is capped at $35, and you do not have to pay a deductible for it. This applies to both Part D and Part B (pump) insulin.
Coverage Limits: How Many Test Strips Can You Get?
Medicare doesn’t give you an unlimited supply of test strips; they have strict “utilization guidelines” based on whether or not you use insulin.
- If You Use Insulin
Because you need to check your sugar more frequently to dose your insulin, Medicare allows for more supplies.
- Limit: Up to 300 test strips and 300 lancets every 3 months.
- Testing Frequency: This assumes you are testing 3 times a day.
- If You Do Not Use Insulin
If you manage diabetes with pills (like Metformin) or diet alone, Medicare covers fewer supplies.
- Limit: Up to 100 test strips and 100 lancets every 3 months.
- Testing Frequency: This assumes you are testing once a day.
“Can I Get More If I Need Them?”
Yes. If your doctor deems it medically necessary for you to test more often—for example, if your blood sugar fluctuates wildly or you are pregnant—they can write a prescription explaining why. You will need to keep a testing log for six months to prove you are actually using the extra supplies.
The "Mail-Order" Myth: Do I Have to Wait for Delivery?
Many New York residents believe they must use a national mail-order company to get their diabetic supplies covered by Medicare. This is not true.
While Medicare has a “National Mail-Order Program” that requires you to use specific suppliers if you want goods shipped to your door, you always have the option to buy locally.
You can walk into a Medicare-enrolled supplier—like a local pharmacy or a medical supply store in Floral Park—and pick up your supplies in person. For many seniors, this is a better option because:
- No Stolen Packages: Porch piracy is a real issue in Queens and NYC.
- Immediate Access: You don’t have to wait 5-7 business days if you run out of strips.
- Customer Service: You can ask a real person how to use your new glucose meter.
At Alfa Healthcare Supply Inc., we specialize in helping locals get the DME they need without the headache of 1-800 numbers.
New for 2025: Continuous Glucose Monitors (CGMs)
Continuous Glucose Monitors (like the Dexcom or FreeStyle Libre) have revolutionized diabetes care. In the past, Medicare coverage for these was very strict. However, guidelines have expanded.
As of 2025, Medicare Part B covers CGMs if:
- You have diabetes (Type 1 or Type 2).
- You use insulin OR you have a history of “problematic hypoglycemia” (low blood sugar events) even if you don’t use insulin.
- Your doctor prescribes it and you see them every 6 months to review your diabetes management.
Pro-Tip for NY Residents: If you are on a Medicare Advantage plan (Part C), coverage might vary slightly, but most plans follow the standard Medicare guidelines. Always check your specific plan’s “Summary of Benefits.”
A Checklist for New York Residents
Navigating insurance in New York can be tricky. Follow this checklist to ensure your supplies are covered:
1. Get a Specific Prescription: A generic note saying “Diabetic Supplies” isn’t enough. Your doctor must write a prescription that includes:
- “Diabetes Mellitus” diagnosis code.
- Whether you use insulin.
- The specific item (e.g., “Glucose Test Strips”).
- Frequency of use (e.g., “Test 3 times daily”).
- Quantity to be dispensed.
2. Check Your Supplier: Ensure you are buying from a Medicare-enrolled supplier. If you buy from a supplier who isn’t enrolled, Medicare will not pay a cent, and you will be stuck with the full bill.
3. Ask About “Assignment”: You want a supplier who “accepts assignment.” This means they agree to the Medicare-approved price. If they don’t, they can charge you “Excess Charges” (up to 15% more).
4. Keep Your Testing Logs: If you are requesting extra supplies above the standard limits, keep a written log of your blood sugar readings. Medicare audits these frequently.
Local Support in Floral Park & Queens
Why deal with faceless call centers when you can get personalized care right here in your neighborhood?
Alfa Healthcare Supply Inc. is dedicated to serving the Floral Park and greater New York community. We understand the nuances of local insurance plans and can help guide you toward the right products for your needs.
Whether you need a new Glucometer, a restock of Test Strips, or are looking into Diabetic Shoes to protect your feet, we are here to help.
Shop Our Diabetic Care Collection Here:/products/diabetic-supplies/
Frequently Asked Questions (FAQs)
Q: Does Medicare cover diabetic socks?
A: Generally, no. Medicare does not cover diabetic socks for the general diabetic population. However, if you have a venous stasis ulcer or other specific wounds, they might be covered as “wound dressings,” but this is rare. Medicare does cover diabetic shoes and inserts once per year if you have qualified foot conditions.
Q: I have both Medicare and Medicaid (Dual Eligible). Do I pay anything?
A: In New York, if you have both Medicare and Medicaid (full coverage), Medicaid usually covers the 20% coinsurance that Medicare leaves behind. This means your cost for diabetic supplies could be $0. Be sure to show both cards to your supplier.
Q: Can I switch from mail-order back to a local store?
A: Yes! You are not locked into a mail-order contract forever. You can choose to pick up your next prescription at a local participating supplier whenever you choose.
Disclaimer: This guide is for informational purposes only and does not constitute medical or legal advice. Medicare guidelines are subject to change. Please verify your specific coverage with Medicare.gov or your plan provider.